
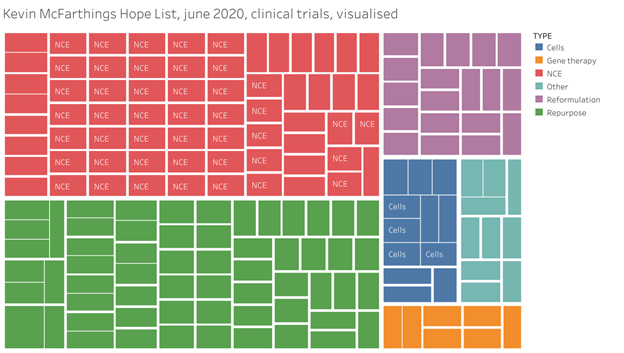
There are currently 77 clinical trials evaluating medications aimed at slowing the progression of Parkinson’s disease. On the surface that sounds like good reason to be optimistic that one of those will strike gold and we will finally have the long sought-after disease modifying therapy for Parkinson’s disease.
Here is an overview of all trials in Parkinson’s at various stages of clinical development…
That picture would seem quite the achievement for the field, especially when one considers how difficult it is for a therapy to get to trial in the first place. First, a researcher has to have an idea about a mechanism of action that seems to be problematic in people with the disease, which itself requires decades spent studying the disease and climbing the ranks to become a scientist. Then they have to get the funding needed to spend years running an experiment that can show some quantifiable benefit in usually two or more of the models we have of Parkinson’s disease. Then they often have to get more funding to demonstrate the therapy can enter the brain and prove to the FDA that it is reasonably safe for humans, usually requiring a few more years of experiments in animals. Then they have to convince someone to give them even more money so they can start testing it in people. And that is just to get to the first clinical trial phase, getting through the various clinical phases can itself be a herculean effort.
So, it seems an impressive feat that we have gotten to the point of having 77 therapies make it this far. It would also seem to indicate that there is a lot of good reason to be hopeful that soon we will have a disease modifying therapy for Parkinson’s disease. Just think about all the people and all the money that had to be involved in getting all those trials to where they are today.
However, once you peel back each layer of each step mentioned above and peer into the grimy details you start to see some fatal flaws in almost every single one of those 77 trials, trials that millions of people around the world have pinned their hopes to.
To begin, the models on which we tested each of these therapies don’t recapitulate the type of Parkinson’s disease that the individuals participating in the clinical trials have. The models, which tend to be hundreds of identical genetically engineered mice or rows of dishes with thousands of perturbed cells in each, usually only mimic some of the cellular destruction or protein aggregation found in dead brains of a small percentage of people diagnosed with Parkinson’s. These models have allowed us to answer very specific questions about our framework of disease, but they do not capture the individual complexity of how what we call Parkinson’s manifests in a given person diagnosed with this disease.
In addition, due to the nature of the publishing industry in science and the business of securing grants to fund large laboratories, too many researchers just focus on developing therapies that can get passed the models, for once they do they can then be sold off or picked up by another entity who is then responsible for getting it across the next flag stick. But there is an even bigger problem with the 77 trials – they have been built on stories we tell each other about what this disease is. Stories about misfolded proteins, aberrant cellular pathways, genetic indicators from genome wide association studies, and much more. These stories are logical and compelling, giving us clues on what we could target in our goal to slow the progression in everyone. These stories, and the evidence we have for an alternate interpretation of the source data, are the subject of Brain Fables. Told through the lens of a doctor and a patient, the parallel narratives that make up the book question the limits of old frameworks that have driven investigations into neurodegenerative diseases for decades, and the frustrations of a young patient advocate who travelled the world looking for solutions to the disease slowly gnawing away at his brain.
Latest Comments
Have your say!