
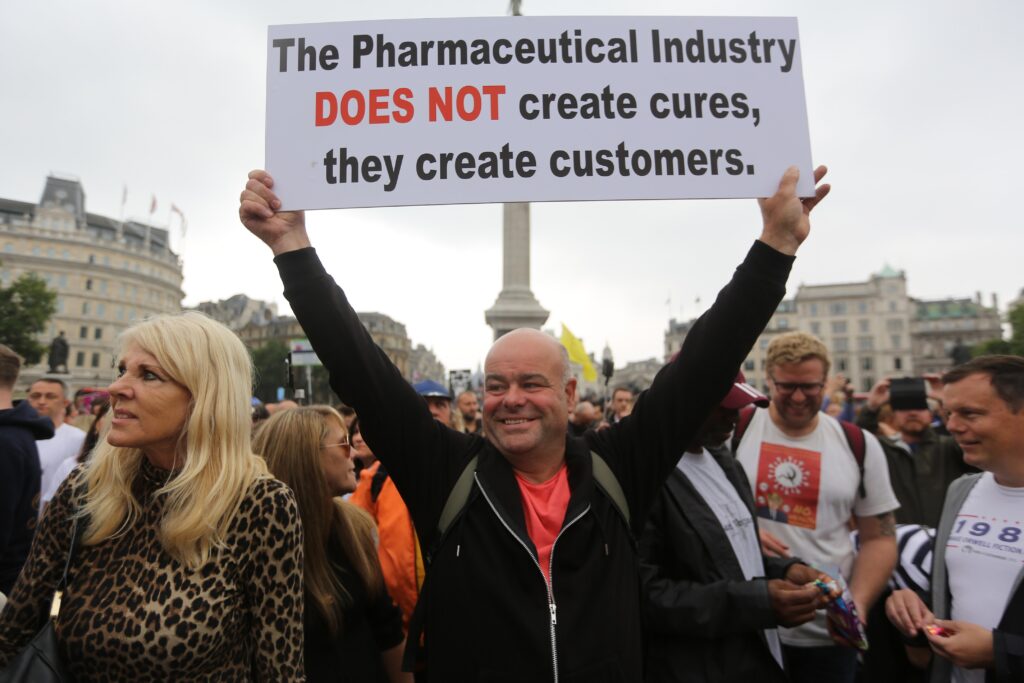
Is vaccine hesitancy purely irrational? Are there good reasons for refusing to wear a face mask? These are some of the questions we address in our forthcoming book Rethinking Evidence in the Time of Pandemics: Scientific vs Narrative Rationality and Medical Knowledge Practices (Cambridge University Press, 2022).
Situated epistemologies
The COVID-19 crisis has transformed the highly specialized issue of what constitutes reliable medical evidence into a topic of public concern. For several months, newspapers and social media abounded with discussions about whether the evidence for wearing masks was weak or strong, or whether mass public health measures such as lockdowns or school closures were backed by sufficient evidence.
Underpinning most of these and other approaches to evidence is however a shared assumption: that evidence is singular and that it can be ranked on a singular scale as present or absent, strong or weak, from a purely rational, value-free perspective.
As an alternative to this singular epistemology underpinning evidence-based medicine, our book argues the need for situated epistemologies that are relative to the site or discourse where the knowledge is articulated and to the narrative location of those who articulate or evaluate that knowledge. Rather than taking the Evidence-Based Medicine (EBM) principles for granted as the only rational means of assessing evidence, we explore the various stories about COVID-19, and offer a theoretical basis for understanding how different individuals and communities decide which of a range of competing stories they should believe in and why.
We believe that it is only by creating awareness about the specific values people adhere to and invest in their narratives that we can adequately understand why they believe in these particular stories.
The Narrative Paradigm
The theoretical framework we apply is Walter Fisher’s narrative paradigm. The basic assumption underpinning the narrative paradigm is that “[n]o matter how strictly a case is argued – scientifically, philosophically, or legally – it will always be a story, an interpretation of some aspect of the world that is historically and culturally grounded and shaped by human personality” (Fisher 1987:49). There is no story, no matter how scientific, that ends all story-telling.
When the proponents of evidence-based medicine talk about critical appraisal of evidence – and whether the evidence is weak or strong – their view is embedded within a rational world paradigm in which the world is conceived as a set of facts and logical puzzles that can be solved through appropriate methods and the application of reason. Our claim is that such appraisal is incomplete. The question ‘what are the facts’ must be supplemented with another one: ‘how do these facts make sense to people, and why’. The latter is not about appraising the facts but about appraising the stories within which they are woven and acquire meaning.
Importantly, we do not reject the EBM paradigm, nor do we suggest that it should be replaced by the narrative paradigm. We merely argue that – from the perspective of the narrative paradigm – the empiricist notion of evidence underpinning EBM is only one possible situated interpretation or value according to which knowledge claims can be and are in practice assessed.
The main purpose of Fisher’s narrative paradigm is to provide a theoretical framework that can account for the way in which any communicative encounter – whether it involves a scientific theory, a fictional story, or a factual account – is assessed by different individuals with different life experiences and values, not by resort to logical inference but on the basis of what he calls “good reason”.
Narrative probability and fidelity
The two principles that define narrative rationality and embody the logic of good reasons in Fisher’s paradigm are narrative probability (what constitutes a coherent story) and, narrative fidelity (whether a story resonates with the audience’s experience and values). These may be thought of as tests that we apply – whether instinctively or through conscious reasoning – to decide whether a narrative offers good reasons for action and belief.
The first test asks whether the story ‘hangs together’. In the context of the pandemic, it isn’t difficult to find stories that don’t. Within the space of nine months, advice issued by the WHO changed from warning against the risk of community masking to encouraging its use. Yet, the theory underpinning the advice was never corrected. Fisher would consider this incoherence as weakness in their practice of evidencing; their story doesn’t hang together.
The second test is about assessing whether the story has ‘truth-qualities’ and ‘rings true’ to the reader. Fidelity does not require the audience to actually share the experiences of protagonists such as black populations and their reasons for a lack of trust in health authorities during the pandemic. It merely requires that these protagonists’ experiences appear to the audience to be ‘true to life – in principle’ (Fisher 1987:176). Even a fictional story can be “true to life – in principle” in the sense of accounting for experiences that seem real or credible “given the universe in which the characters live and the logic of their story” (Fisher 1987:176).
In an article in the Conversation from January 2021, Winston Morgan, a reader in toxicology and clinical biochemistry, uses the example of vaccine hesitancy among black communities in the early phase of the pandemic. In the first wave of the pandemic, when the virus was shown to be affecting certain ethnic groups more than others, one solution proposed by the medical profession was to start the vaccine roll out with the most vulnerable communities, including people from Black, Asian and minority ethnic groups. However:
This caused concern among these communities, because they are not normally at the front of the queue when it comes to the best medical treatments, particularly those in lower socioeconomic classes. Some people began to speculate that it was because it was an experimental vaccine and Black people were being used as guinea pigs.
This may not be true, but it was definitely true to life for many of the people who identified with these stories.
To conclude, we believe that the concerns of those who object to various restrictions such as wearing face masks or are vaccine-hesitant can only be addressed and contested by understanding and engaging with the logics of the stories to which they subscribe.
Latest Comments
Have your say!